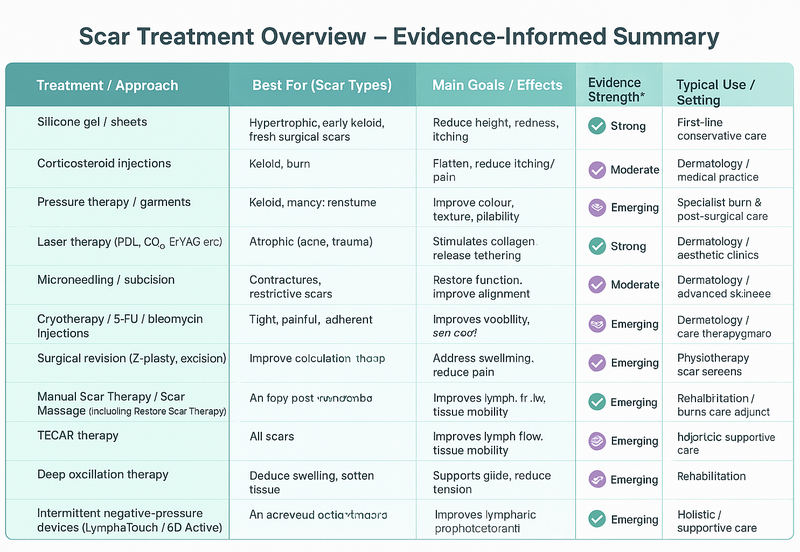
Effective scar management integrates biomechanical, sensory, and aesthetic considerations. Treatment choice should reflect scar type, depth, stage of healing, and patient goals. Intervention may be medical, procedural, or manual, and outcomes improve when techniques are multimodal and collaborative.
STANDARD / EVIDENCE BASED SCAR TREATMENTS
TOPICAL AGENTS
What They Are:
Creams, gels, or silicone-based products applied to the skin.
Examples:
-
Silicone gel/sheets: help flatten and soften raised scars (keloid and hypertrophic).
-
Moisturising creams and oils: support healing and reduce dryness or itching.
-
Prescription creams: may contain mild steroids or retinoids to reduce redness or stimulate new collagen.
- Pressure therapy: established for burn scars; evidence moderate but long-standing clinical consensus.
Best For:
Fresh scars, hypertrophic scars, minor surgical or injury scars, burns.
INJECTABLES AND MEDICAL TREATMENTS
What They Are:
Treatments performed by medical professionals to change scar tissue structure or reduce symptoms.
Examples:
- Intralesional corticosteroids (triamcinolone): reduce collagen synthesis and pruritus in hypertrophic/keloid scars.
-
Laser therapy (PDL, fractional CO₂, Er:YAG): improves colour, pliability, and patient-reported outcomes; supported by multiple RCTs.
-
Microneedling / subcision: stimulate neocollagenesis and release tethering in atrophic or adherent scars.
-
Cryotherapy / 5-FU / bleomycin: adjuncts for refractory keloids.
Best For:
Keloid and hypertrophic scars, atrophic (pitted) scars, or scars that are red, thick, or raised.
SURGICAL AND PROCEDURAL TREATMENTS
What They Are:
Surgical scar revision or other procedures designed to release or remove problematic tissue.
Examples:
-
Scar revision surgery: removes old scar tissue and repositions the skin for better healing.
-
Punch excision / subcision: lifts or releases deep, tethered scars (e.g., acne or burn scars).
-
Laser resurfacing or microneedling: encourages collagen renewal and improves skin texture.
Best For:
Severely tight, sunken, or distorted scars; scars restricting movement; complex surgical scars.
MANUAL AND FUNCTIONAL INTERVENTIONS
Scars can create restrictions that extend beyond the visible surface, involving deeper fascial, muscular, and connective tissue layers.
These restrictions may alter movement, posture, or load transfer, and in some cases influence visceral mobility, particularly in abdominal or large surgical scars.
Manual and movement-based therapies aim to restore tissue glide, comfort, and functional movement by addressing both local and systemic effects.
MANUAL SCAR THERAPY
What it is:
A targeted, hands-on approach designed to mobilise superficial and deep scar tissue, fascia, and surrounding structures.
What it’s best for:
Scars that present with tightness, restriction, or pain — especially following surgery, trauma, or burns.
How it helps:
Techniques focus on improving tissue elasticity, reducing adhesions, and modulating sensory feedback. Manual Scar Therapy can enhance range of motion, reduce hypersensitivity, and improve local circulation. Evidence is emerging from case studies and pilot trials showing improved mobility and patient-reported comfort.
SCAR MASSAGE
What it is:
A foundational conservative technique using controlled manual pressure and directional strokes to remodel scar tissue.
What it’s best for:
Mature scars with superficial stiffness or sensory changes; ideal for patient self-management under professional guidance.
How it helps:
Encourages collagen realignment, improves hydration, and desensitises the area. When combined with other modalities (e.g., silicone, laser, or movement therapy), it supports long-term scar remodelling and improved tactile comfort.
RESTORE SCAR THERAPY
What it is:
An integrative manual therapy system addressing both the superficial and deep fascial layers, combining elements of myofascial release, connective tissue work, and neurosensory retraining.
What it’s best for:
Complex or restrictive scars that affect range of motion, posture, or sensory feedback — particularly abdominal, orthopaedic, or reconstructive scars.
How it helps:
Targets fascial restrictions, neural tension, and proprioceptive imbalances. Clinical outcomes include improved tissue glide, reduced pain, and enhanced movement efficiency. Evidence is currently emerging from practice-based case studies and early clinical research.
PHYSIOTHERAPY & MOVEMENT REEDUCATION
What it is:
Functional rehabilitation integrating mobility, strengthening, posture correction, and proprioceptive training to address compensatory patterns resulting from scarring.
What it’s best for:
Scars that restrict joint mobility, affect gait or posture, or contribute to chronic pain syndromes.
How it helps:
Restores movement symmetry, improves load distribution, and reduces secondary dysfunction caused by fascial or scar-related tension. Physiotherapy complements manual scar interventions and supports long-term functional recovery.
ADJUNCT DEVICE- AND TAPE- BASED OPTIONS
Scars can create restrictions that extend beyond the visible surface, involving deeper fascial, muscular, and connective tissue layers.
These restrictions may alter movement, posture, or load transfer, and in some cases influence visceral mobility, particularly in abdominal or large surgical scars.
Manual and movement-based therapies aim to restore tissue glide, comfort, and functional movement by addressing both local and systemic effects.
T.E.C.A.R. THERAPY
Mechanism:
Deep thermal/electromagnetic stimulation to increase perfusion and reduce nociception.
Evidence:
Emerging RCTs and clinical series show benefits for pain and early remodelling; high-quality trials specifically for scar cosmetic outcomes remain limited.
Indications:
Consider TECAR to reduce pain and facilitate early mobilisation when used with manual scar therapy.
DEEP OSCILATION
Mechanism:
Micro-oscillatory tissue movement with reported anti-inflammatory and lymphatic effects.
Evidence:
Case series and small trials (burns, post-op) suggest reduced oedema and improved scar pliability; larger RCTs are sparse.
Indications:
Useful adjunct for oedematous/early remodelling scars.
NEGATIVE PRESSURE DEVICES
Mechanism:
Controlled suction and mechano-transduction to promote lymphatic return and tissue glide.
Evidence:
NPT is proven for wound healing; newer intermittent negative-pressure devices show promising pilot/clinical studies for improving lymphatic flow and scar mobility but long-term cosmetic evidence is limited.
Indications:
Use for adherent, oedematous or lymphatic-compromised scars alongside manual lymphatic drainage.
KINESIOTAPING
Mechanism:
Reduce shear/tension across scar, support tissue glide, provide proprioceptive input.
Evidence:
Multiple trials/reviews report improvements in scar pliability, colour and symptoms when combined with other therapies.
Indications:
Often used to support rehabilitation and offload skin under tension.
EVIDENCE LANDSCAPE
Until recently, most scar research focused on burn scars, where long-term outcomes are easily measured. Over the past decade, studies have expanded to include surgical, traumatic, acne and aesthetic scars, and the quality of evidence is steadily improving.
Strong evidence supports silicone, steroid injections, and several laser and microneedling protocols. Manual scar therapy, TECAR, deep oscillation, negative pressure, and kinesiotaping are evidence-informed adjuncts: they show promising clinical outcomes for pain, oedema, and mobility, but large, high-quality trials are still needed to confirm long-term remodeling effects.
In short: scar treatment research is evolving — evidence is growing but not yet complete — and outcomes are best when therapies are combined and tailored to the individual.