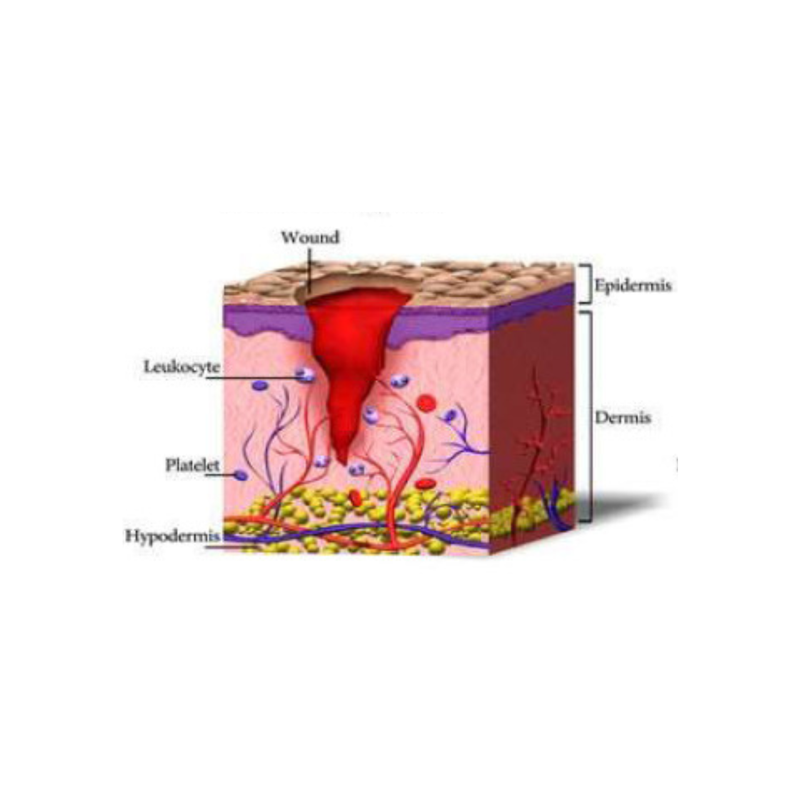
Wound healing is a complex, multi-phase process involving cellular, molecular, and mechanical events. Most scars follow a predictable healing pathway, but some factors can lead to pathological scarring (hypertrophic or keloid). Below is a more detailed look at the healing stages and what distinguishes ‘normal’ from pathological scar development.
STAGES OF WOUND HEALING AND SCAR FORMATION
2. INFLAMMATION
- Neutrophils arrive first, followed by macrophages; these remove bacteria, debris.
-
Macrophages release cytokines, growth factors that attract fibroblasts and initiate tissue repair.
-
The extent and duration of inflammation are critical: prolonged or excessive inflammation can predispose to pathological scarring.
- Starts within 24-48 hours and lasts up to 4-7 days
3. PROLIFERATION
- Fibroblasts migrate in, secrete extracellular matrix (ECM) including collagen (initially more type III), glycosaminoglycans; angiogenesis (new blood vessel formation), epithelialisation.
-
Granulation tissue forms.
-
Myofibroblasts appear: help contract wound edges.
- Starts around day 4 and last around 21 days
4. MATURATION
- Gradual replacement of collagen III with collagen I, reorientation of collagen fibres, reduction in cellularity and vascularity.
- Myofibroblasts undergo apoptosis, ECM turnover balances .
- Scar becomes softer, flatter, less red; tensile strength improves, but rarely reaches that of uninjured skin fully.
- Starts around day 21 and can last for months or even years.

FACTORS INFLUENCING SCAR FORMATION AND HEALING
- Size and depth of the wound – The extent of tissue damage determines the degree of inflammation, fibroblast activity, and collagen deposition. Deeper or larger wounds involve dermal structures and take longer to remodel, increasing the likelihood of visible or restrictive scarring.
- Location on the body – Areas subject to high tension, shear, or frequent movement (such as joints, shoulders, or sternum) are more prone to hypertrophic scarring. Regional variations in blood supply, skin thickness, and mechanical load also influence collagen alignment and remodelling.
- Wound management – Optimal wound closure, moisture balance, and early protection of new epithelial tissue support organised collagen deposition. Conversely, poor dressing choice, desiccation, or excessive mechanical stress can promote delayed healing and fibrosis.
- Infection or delayed healing – Infection prolongs the inflammatory phase and increases cytokine and fibroblast activation, which may lead to excessive collagen synthesis and abnormal scarring.
- Skin type and tone – Fitzpatrick skin types IV–VI have a higher incidence of keloid formation, likely due to increased fibroblast reactivity and melanocytic response. Pigmentation changes and post-inflammatory hyperpigmentation may also be more prominent.
- Age – Younger individuals demonstrate faster cellular turnover and stronger inflammatory and fibroblastic responses, predisposing to more noticeable scarring. In contrast, older skin heals more slowly with less robust collagen synthesis but tends to scar less prominently.
- Genetic and familial predisposition – Keloid and hypertrophic scar formation show familial clustering and ethnic predilection, with known associations to certain HLA subtypes and TGF-β pathway polymorphisms.
- Systemic health and nutrition – Chronic illnesses (e.g., diabetes, vascular disease) and nutritional deficiencies (vitamin C, zinc, protein) impair collagen synthesis and angiogenesis, delaying healing and affecting scar quality.
- Mechanical stress and repeated trauma – Ongoing friction, stretch, or impact at the wound site maintains fibroblast activation and disrupts remodelling, perpetuating hypertrophic or adherent scarring.
- Medications and local factors – Corticosteroids, anticoagulants, or certain chemotherapeutic agents can influence tissue repair. Radiation or prior inflammation in the area may reduce vascularity and impair healing capacity.
Understanding the factors that influence scar formation helps therapists identify potential risks early and adapt treatment accordingly. Considering wound depth, tissue tension, systemic health, and client-specific variables allows for a more individualised approach — optimising outcomes, minimising complications, and supporting effective, comfortable recovery.
PATHOLOGICAL SCARS
Pathological scarring arises from abnormal wound healing characterized by excessive fibroblast activity and collagen deposition. This leads to thickened, raised, and sometimes functionally or cosmetically problematic scars. The two principal forms are hypertrophic scars and keloids, which share overlapping mechanisms but differ in clinical behaviour and response to treatment.
(References: Ogawa 2017; Niessen et al. 1999; Trace et al. 2016)
Hypertrophic scars are erythematous, raised lesions that remain confined within the original wound boundaries. They typically develop within 4–8 weeks post-injury, often in areas of high tension or after burns.
(Atiyeh et al. 2005)
Pathophysiology:
These scars result from prolonged inflammation and mechanical tension, which stimulate fibroblast proliferation and type III collagen overproduction. Unlike keloids, collagen fibers are organized parallel to the skin surface and tend to remodel over time.
(Tredget et al. 2009)
Prevention:
Optimal surgical techniques minimizing tension, early silicone gel/sheet application, and pressure garments (15–25 mmHg) are proven preventive measures.
(Ogawa 2017; Mustoe et al. 2002)
Treatment:
-
First-line: Silicone therapy and pressure garments.
-
Adjuncts: Intralesional corticosteroids (e.g., triamcinolone), pulsed dye laser (PDL), and fractional CO₂ laser.
-
Refractory cases: Surgical excision with postoperative silicone/pressure therapy or combination with corticosteroids.
(Sharpe et al. 2020; Ogawa 2017)
Keloids are benign fibroproliferative growths extending beyond the original wound borders, often continuing to grow for years. They occur more frequently in individuals with darker Fitzpatrick skin types (III–VI) and have a strong genetic component.
(Bayat et al. 2003)
Pathophysiology:
Keloids exhibit dysregulated wound healing characterized by persistent fibroblast activation, reduced apoptosis, and excessive type I and III collagen production arranged haphazardly. Cytokines such as TGF-β1 and PDGF play central roles.
(Slemp & Kirschner 2006; Limandjaja et al. 2020)
Prevention:
High-risk patients should avoid unnecessary trauma, piercings, or elective surgery in predisposed regions. Early application of silicone sheets or pressure therapy following wound closure can reduce keloid formation.
(Ogawa 2017; Mustoe et al. 2002)
Treatment:
Effective management often requires multimodal therapy:
-
Intralesional corticosteroids (triamcinolone acetonide 10–40 mg/mL) remain first-line.
-
Adjuncts: Cryotherapy, 5-fluorouracil or bleomycin injections, laser therapy (PDL or Nd:YAG), and interferon-α/γ.
-
Surgical excision should always be combined with adjuvant radiotherapy or steroid injections to minimize recurrence (which can reach 45–100% without adjuvant therapy).
(Ogawa 2017; Al-Attar et al. 2006)
Key References
-
Ogawa R. Keloid and hypertrophic scars are the result of chronic inflammation in the reticular dermis. Inflamm Regen. 2017.
-
Mustoe TA et al. International clinical recommendations on scar management. Plast Reconstr Surg. 2002.
-
Atiyeh BS et al. Hypertrophic scars and keloids: pathophysiology and management. Clin Plast Surg. 2005.
-
Al-Attar A et al. Keloid pathogenesis and management: review of the literature. J Plast Reconstr Aesthet Surg. 2006.
-
Limandjaja GC et al. The keloid disorder: heterogeneity, histopathology, and pathogenesis. Exp Dermatol. 2020.

FUNCTIONAL AND DEEP EFFECTS OF SCARING
BEYOND PATHOLOGICAL SCAR
Not all problematic scars meet the criteria for pathological hypertrophy or keloid formation. Many remain histologically “normal” yet cause functional, sensory, or biomechanical disturbances that persist long after epithelial closure.
The visible scar represents only a fraction of the tissue changes. Deep to the skin, remodeling occurs within the subcutaneous tissue, fascia, and myofascial planes, influencing tissue glide, neurosensory feedback, and load distribution.
Because fascia forms a continuous network through the body, restrictions in one area may produce pain, altered movement patterns, or compensatory dysfunction elsewhere. (Findley & Schleip 2007; Stecco et al. 2013)
In regions such as the abdomen and pelvis, post-surgical adhesions and fascial tension can contribute to visceral symptoms, including gastrointestinal discomfort or reproductive pain, by altering fascial slide and autonomic regulation. (Bordoni & Zanier 2014; Hodges et al. 2019)
A comprehensive approach to scar assessment therefore includes evaluation of movement, tissue mobility, posture, and sensory feedback, not just scar appearance.
TYPES OF NON-PATHOLOGICAL BUT PROBLEMATIC SCARS
ATROPHIC SCARS
Atrophic scars are characterized by dermal thinning and loss of underlying tissue volume, leading to a depressed or pitted appearance.
Common in acne, varicella, or post-surgical wounds with poor dermal regeneration.
Pathophysiology:
Insufficient fibroblast activity or degradation of extracellular matrix exceeds collagen synthesis during healing.
(Alster & Lupton 2003)
Management:
-
Minimally invasive: Microneedling, fractional laser resurfacing, and chemical peels stimulate neocollagenesis.
-
Augmentative: Dermal fillers (e.g., hyaluronic acid) or autologous fat grafting restore volume.
-
Topical adjuncts: Retinoids and growth factor–based treatments.
CONTRACTED SCARS
Linear or band-like scarring resulting in soft tissue contracture and functional limitation, particularly over joints or high-tension areas.
Mechanism:
Myofibroblast activity during remodelling phase drives excessive contraction. Chronic tension perpetuates fibrosis.
(Desmoulière et al. 2005)
Management:
-
Early mobilization and stretching post-closure.
-
Silicone gel sheets, pressure garments, and manual scar therapy to maintain tissue pliability.
-
Laser or surgical release when dense fibrous bands restrict motion.
CORDING SCAR BANDS
Palpable, tight subcutaneous cords, often post-axillary or breast surgery, sometimes extending down the arm.
(Ozmen et al. 2016)
Pathophysiology:
Believed to arise from thrombosed lymphatic channels or fibrosed fascial planes tethered by healing scar tissue.
Management:
-
Physiotherapy and manual lymphatic techniques to gradually restore range of motion.
- manual scar massage techniques (Restore works really well)
-
Low-level laser therapy (LLLT) and gentle stretching shown to reduce pain and tension.
(Nedelec et al. 2012)
ADHESIONS
Abnormal fibrous connections between scar tissue and underlying fascia, muscles, or visceral layers.
Pathophysiology:
Impaired collagen remodelling leads to loss of gliding surfaces and fixation between adjacent structures.
(Bennett et al. 2010)
Clinical Presentation:
Restricted movement, pain, altered sensation, or “dragging” sensations along scar lines or deeper planes.
Management:
-
Manual scar mobilization, instrument-assisted soft tissue therapy, and graded movement re-education.
-
In refractory cases: adhesiolysis or subcision.
Prevention:
Early movement and controlled mechanical loading during maturation phase.
Selected References
-
Findley TW, Schleip R. Fascia research: a narrative review. J Bodyw Mov Ther. 2007.
-
Stecco C et al. The fascial system and its role in wound healing and scar formation. Clin Anat. 2013.
-
Bordoni B, Zanier E. Abdominal scars and their influence on the body system: a fascial perspective. J Multidiscip Healthc. 2014.
-
Hodges PW et al. Interrelationship of the abdominal wall, diaphragm, and pelvic floor muscles. Neurourol Urodyn. 2019.
-
Alster TS, Lupton JR. Improvement of atrophic facial scars with nonablative laser therapy. Dermatol Surg. 2003.
-
Desmoulière A et al. Myofibroblasts and mechanotransduction in pathological remodeling. Lab Invest. 2005.
-
Ozmen T et al. Axillary web syndrome: current understanding and management. Breast Care. 2016.
-
Bennett G et al. Adhesions and scar management after surgery: a review. J Wound Care. 2010.
CLINICAL TAKEAWAY
Scars should be assessed as part of a whole-body system. Superficial healing does not necessarily indicate functional recovery. Integrating manual therapy, fascial release, and neuromuscular re-education into scar management enhances outcomes and helps restore dynamic balance and movement efficiency.